Calling all Healthcare providers to go viral
March 31, 2020Hello Doctor, Can I Interest
You In A Pamphlet?
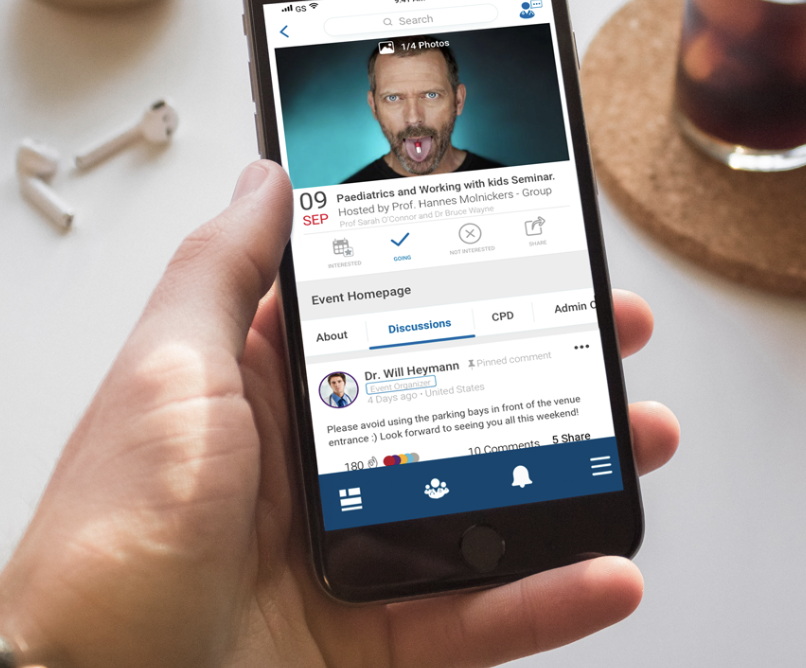
Stay connected with your healthcare community
through MediFellows blog
Hello Doctor, Can I Interest You In A Pamphlet?
Stay connected with your healthc are community through MediFellows blog
October 21, 2019
My stream of consciousness around tech and burnout in the Healthcare Industry.
Not only is the healthcare industry a digital laggard: riddled with inefficiencies; impersonal care, old technologies, and siloed digital approaches; it is also inherently averse to change – being highly regulated, with sensitivities around security and privacy of information.
I recently took to LinkedIn in an attempt to encourage meaningful communication between myself and like-minded professionals in the healthcare industry.
I was a rep once, so I eagerly searched the platform for my doctors, pharmacists and others I’d engaged with in the past... but, hardly anyone I searched for came up... Ok, well, I’d also engaged with numerous healthcare associations, institutions and practices in my marketing capacity, so I searched for these. Again, limited results…
I began to question my search method. The bottom line was a dismal attendance; not surprising, given the pace of the average Healthcare Professional’s (HCP) life.
Resource overload
As with any industry, an exchange of information is imperative. Time, by far, is the HCP’s most scarce resource, so it is understandable that it can become a nightmare when trying to determine which sources of information are the most meaningful and credible.
After all, we are bombarded with a multitude of options: conferences, CMEs, research, studies, journal clubs, websites, drug interaction checkers, acute and chronic medical aid references, prescription dosing, indications… the list goes on and on.
Then there is the time required for other administrative tasks that are often not attended to. The annual Russian Roulette of whose CPD (continual professional development) points will be audited when the time comes, is never pleasant to watch. The paradox that digitising electronic health records, should be making the healthcare professionals lives easier, is sadly ironic as it continues to attribute to physician burn out.
The amount of clerical and administrative work required for payers and other stakeholders, continues to compromise the patient. It results in less time with the patient and strangleholds what is left of the physician's autonomy and time.
As if this isn’t enough, there is also the obligatory industry airtime the HCPs are required to give:
* Sales reps in-practice
* The cumulative hours spent walking around industry exhibitions (whose headline acts are showers of branded pens)
* Publications oversaturated with advertisements (depending on the publication, one has to question the credibility of the journalism and editorials which, more and more, are reading suspiciously like advertorials).
These are just a few of the tactics in the pharmaceutical marketing arsenal, and after years of repetition, a lot of information portrayed is met with skepticism.
Across the board, the age-old model of pharmaceutical marketing is stale and uninspired in this day and age. However, budgets are needed for the support of the profession. The company that opts not to engage in these antiquated activities, appears more conspicuous by absence. It’s such a pity when there are more efficient ways to have meaningful conversations with clients - especially in the digital era.
HCPs are burnt out, information exchange is inefficient, and industry is not doing anything disruptive enough to shift the status quo.
Why is this industry, in particular, not embracing the information sharing and crowd-sourcing benefits of the digital age, that is enjoyed by so many other industries?
Digital Deep Dive
Beside the obvious PTSD of their ‘technology’ experiences with Electronic Health Records (EHRs), this conundrum has been hounding me. I heard the plight of the healthcare professional amidst the frustration of being a marketer in a space where there are significant budgets, enormous clout amongst established industry leaders, and less and less airtime with clients.
I have always taken on my professional role with my clients, products and teams as personally, and with the same anxious enthusiasm, as I would my own child. So I leapt into research, a lot of it. Being the millennial that I am (yes, I just make the cut!) I did a digital deep-dive. As you would imagine, there are some incredibly insightful pieces and conversations one can have in this digital age, when you ask the right questions, using the right platforms.
Which brings me to a statistic that completely took me aback. Recent research has revealed that almost 90% of hospitals in America still rely on pagers, considering them to be more secure, compared to smartphone-based communication. I read the same sentence over and over, until I was certain I hadn’t misread anything. Are we really using an analogue technology in the “mHealth” (Mobile Health) era?
The article goes on to clarify that outmoded modes of communication (like pagers) are far less efficient and estimated to cost US hospitals $8.3 billion a year in reduced productivity! Naturally, this then also impacts on quality of care as it takes away from the time that can be spent interfacing directly with patients. This not only highlights the inherently glacial pace of communication technology adoption in healthcare, but also represents an opportunity for new products that specifically address the unique challenges of the industry.
The majority of resources I identified for the clinician were primarily offline, however there were initiatives slowly coming online.
In South Africa, my stomping ground, there are conferences, journals, CPDs, and other resources taking these steps. They are not being executed especially well, and are happening at a snail’s pace, but at least there are websites and even social media pages, on existing public platforms. I saw a scary number of text heavy, WordPress websites, with poor user experiences, little detail, and easily hackable login portals (almost every login registration requirement being different from the next). I discovered a handful of apps, all with different siloed solutions, which creates a disjointed and confusing experience (and again, with differing login requirements).
Industry websites and apps are better developed and managed, however these always appear to be laden with the commercial agenda that their shareholders require. Understandably, as much as the Florence Nightingale persona establishes brand loyalty, there are commercial objectives to fulfil.
Still, it makes the HCP think before registering on a database that will be mined in exchange for the use of this service. I recently had a meeting with a significantly influential government body in the healthcare space. I was told that the application programming interface API (a software interface that allows applications to talk to each other) for their website is “still being developed” and has been at that stage for over a year. Sigh ...
So, from both the public and private sectors, I am not seeing a smooth transition to a more digitized healthcare ecosystem. The result is not surprising: Non-compliance - ironically, the term that makes every HCP shudder.
An international search reveals the contrast one would expect when comparing the digital developments of first-world and third-world countries. There are some amazing online tools that ‘get’ the digital revolution. The ubiquitous use of "Health Tech” and "Health 2.0” conjures up images of artificial intelligence (AI), virtual reality and intimidatingly ambitious tech devices that can diagnose, monitor, treat and even cure disease. There are already murmurings of the “Health 3.0” revolution.
And now?
But what about now? There is a proliferation of patient-centric technology, but what about the Healthcare Professionals? Where are the meaningful, cross-disciplinary conversations taking place? Why is everyone working in silos? Ironic, given the overuse of the word “Interoperability” – a buzz word that has been ‘making the rounds’ in the healthcare space for some time now – referring, for the most part, to EHRs. Although putting the letter “e” in front of already existing systems does technically make them “digital”, it doesn’t necessarily make them any more efficient or engaging.
Regardless of the reasons, which are complex and justifiable, this is me reaching out to those of you in this sphere, and the reason for what I am doing at MediFellows.
My purpose is to engage with those forward thinkers and digital leaders that are proactive in this space. Let’s exchange feedback, advice, mentorship, and more. I love the industry and my feet are strapped to the pedals on this one.
Published by: Fiona McGuirk
References:
https://www.physiciansweekly.com/wp-content/uploads/2016/08/frustrated-doctor-crazy-1080x663.png
https://www.forbes.com/sites/robertpearl/2019/07/08/physician-burnout-1/#f62ad8d119e8
https://www.capgemini.com/resources/digital-healthcare-survey/
https://www.siemens-healthineers.com/magazine/mso-pulse-plus-survey.html
https://rockhealth.com/why-doctors-still-use-pagers/
https://www.forbes.com/sites/dangingiss/2019/07/10/as-healthcare-goes-digital-consumer-engagement-and-experience-improve/#4996aeb496e6/
https://www.healthleadersmedia.com/clinical-care/3-takeaways-healthleaders-innovation-exchange
https://www.himss.org/news/current-state-interoperability
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5559244/
https://blogs.scientificamerican.com/observations/electronic-health-records-and-doctor-burnout/
Not only is the healthcare industry a digital laggard: riddled with inefficiencies; impersonal care, old technologies, and siloed digital approaches; it is also inherently averse to change – being highly regulated, with sensitivities around security and privacy of information.
I recently took to LinkedIn in an attempt to encourage meaningful communication between myself and like-minded professionals in the healthcare industry.
I was a rep once, so I eagerly searched the platform for my doctors, pharmacists and others I’d engaged with in the past... but, hardly anyone I searched for came up... Ok, well, I’d also engaged with numerous healthcare associations, institutions and practices in my marketing capacity, so I searched for these. Again, limited results…
I began to question my search method. The bottom line was a dismal attendance; not surprising, given the pace of the average Healthcare Professional’s (HCP) life.
Resource overload
As with any industry, an exchange of information is imperative. Time, by far, is the HCP’s most scarce resource, so it is understandable that it can become a nightmare when trying to determine which sources of information are the most meaningful and credible.
After all, we are bombarded with a multitude of options: conferences, CMEs, research, studies, journal clubs, websites, drug interaction checkers, acute and chronic medical aid references, prescription dosing, indications… the list goes on and on.
Then there is the time required for other administrative tasks that are often not attended to. The annual Russian Roulette of whose CPD (continual professional development) points will be audited when the time comes, is never pleasant to watch. The paradox that digitising electronic health records, should be making the healthcare professionals lives easier, is sadly ironic as it continues to attribute to physician burn out.
The amount of clerical and administrative work required for payers and other stakeholders, continues to compromise the patient. It results in less time with the patient and strangleholds what is left of the physician's autonomy and time.
As if this isn’t enough, there is also the obligatory industry airtime the HCPs are required to give:
* Sales reps in-practice
* The cumulative hours spent walking around industry exhibitions (whose headline acts are showers of branded pens)
* Publications oversaturated with advertisements (depending on the publication, one has to question the credibility of the journalism and editorials which, more and more, are reading suspiciously like advertorials).
These are just a few of the tactics in the pharmaceutical marketing arsenal, and after years of repetition, a lot of information portrayed is met with skepticism.
Across the board, the age-old model of pharmaceutical marketing is stale and uninspired in this day and age. However, budgets are needed for the support of the profession. The company that opts not to engage in these antiquated activities, appears more conspicuous by absence. It’s such a pity when there are more efficient ways to have meaningful conversations with clients - especially in the digital era.
HCPs are burnt out, information exchange is inefficient, and industry is not doing anything disruptive enough to shift the status quo.
Why is this industry, in particular, not embracing the information sharing and crowd-sourcing benefits of the digital age, that is enjoyed by so many other industries?
Digital Deep Dive
Beside the obvious PTSD of their ‘technology’ experiences with Electronic Health Records (EHRs), this conundrum has been hounding me. I heard the plight of the healthcare professional amidst the frustration of being a marketer in a space where there are significant budgets, enormous clout amongst established industry leaders, and less and less airtime with clients.
I have always taken on my professional role with my clients, products and teams as personally, and with the same anxious enthusiasm, as I would my own child. So I leapt into research, a lot of it. Being the millennial that I am (yes, I just make the cut!) I did a digital deep-dive. As you would imagine, there are some incredibly insightful pieces and conversations one can have in this digital age, when you ask the right questions, using the right platforms.
Which brings me to a statistic that completely took me aback. Recent research has revealed that almost 90% of hospitals in America still rely on pagers, considering them to be more secure, compared to smartphone-based communication. I read the same sentence over and over, until I was certain I hadn’t misread anything. Are we really using an analogue technology in the “mHealth” (Mobile Health) era?
The article goes on to clarify that outmoded modes of communication (like pagers) are far less efficient and estimated to cost US hospitals $8.3 billion a year in reduced productivity! Naturally, this then also impacts on quality of care as it takes away from the time that can be spent interfacing directly with patients. This not only highlights the inherently glacial pace of communication technology adoption in healthcare, but also represents an opportunity for new products that specifically address the unique challenges of the industry.
The majority of resources I identified for the clinician were primarily offline, however there were initiatives slowly coming online.
In South Africa, my stomping ground, there are conferences, journals, CPDs, and other resources taking these steps. They are not being executed especially well, and are happening at a snail’s pace, but at least there are websites and even social media pages, on existing public platforms. I saw a scary number of text heavy, WordPress websites, with poor user experiences, little detail, and easily hackable login portals (almost every login registration requirement being different from the next). I discovered a handful of apps, all with different siloed solutions, which creates a disjointed and confusing experience (and again, with differing login requirements).
Industry websites and apps are better developed and managed, however these always appear to be laden with the commercial agenda that their shareholders require. Understandably, as much as the Florence Nightingale persona establishes brand loyalty, there are commercial objectives to fulfil.
Still, it makes the HCP think before registering on a database that will be mined in exchange for the use of this service. I recently had a meeting with a significantly influential government body in the healthcare space. I was told that the application programming interface API (a software interface that allows applications to talk to each other) for their website is “still being developed” and has been at that stage for over a year. Sigh ...
So, from both the public and private sectors, I am not seeing a smooth transition to a more digitized healthcare ecosystem. The result is not surprising: Non-compliance - ironically, the term that makes every HCP shudder.
An international search reveals the contrast one would expect when comparing the digital developments of first-world and third-world countries. There are some amazing online tools that ‘get’ the digital revolution. The ubiquitous use of "Health Tech” and "Health 2.0” conjures up images of artificial intelligence (AI), virtual reality and intimidatingly ambitious tech devices that can diagnose, monitor, treat and even cure disease. There are already murmurings of the “Health 3.0” revolution.
And now?
But what about now? There is a proliferation of patient-centric technology, but what about the Healthcare Professionals? Where are the meaningful, cross-disciplinary conversations taking place? Why is everyone working in silos? Ironic, given the overuse of the word “Interoperability” – a buzz word that has been ‘making the rounds’ in the healthcare space for some time now – referring, for the most part, to EHRs. Although putting the letter “e” in front of already existing systems does technically make them “digital”, it doesn’t necessarily make them any more efficient or engaging.
Regardless of the reasons, which are complex and justifiable, this is me reaching out to those of you in this sphere, and the reason for what I am doing at MediFellows.
My purpose is to engage with those forward thinkers and digital leaders that are proactive in this space. Let’s exchange feedback, advice, mentorship, and more. I love the industry and my feet are strapped to the pedals on this one.
Published by: Fiona McGuirk
References:
https://www.physiciansweekly.com/wp-content/uploads/2016/08/frustrated-doctor-crazy-1080x663.png
https://www.forbes.com/sites/robertpearl/2019/07/08/physician-burnout-1/#f62ad8d119e8
https://www.capgemini.com/resources/digital-healthcare-survey/
https://www.siemens-healthineers.com/magazine/mso-pulse-plus-survey.html
https://rockhealth.com/why-doctors-still-use-pagers/
https://www.forbes.com/sites/dangingiss/2019/07/10/as-healthcare-goes-digital-consumer-engagement-and-experience-improve/#4996aeb496e6/
https://www.healthleadersmedia.com/clinical-care/3-takeaways-healthleaders-innovation-exchange
https://www.himss.org/news/current-state-interoperability
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5559244/
https://blogs.scientificamerican.com/observations/electronic-health-records-and-doctor-burnout/
October 21, 2019
My stream of consciousness around tech and burnout in the Healthcare Industry.
Not only is the healthcare industry a digital laggard: riddled with inefficiencies; impersonal care, old technologies, and siloed digital approaches; it is also inherently averse to change – being highly regulated, with sensitivities around security and privacy of information.
I recently took to LinkedIn in an attempt to encourage meaningful communication between myself and like-minded professionals in the healthcare industry.
I was a rep once, so I eagerly searched the platform for my doctors, pharmacists and others I’d engaged with in the past... but, hardly anyone I searched for came up... Ok, well, I’d also engaged with numerous healthcare associations, institutions and practices in my marketing capacity, so I searched for these. Again, limited results…
I began to question my search method. The bottom line was a dismal attendance; not surprising, given the pace of the average Healthcare Professional’s (HCP) life.
Resource overload
As with any industry, an exchange of information is imperative. Time, by far, is the HCP’s most scarce resource, so it is understandable that it can become a nightmare when trying to determine which sources of information are the most meaningful and credible.
After all, we are bombarded with a multitude of options: conferences, CMEs, research, studies, journal clubs, websites, drug interaction checkers, acute and chronic medical aid references, prescription dosing, indications… the list goes on and on.
Then there is the time required for other administrative tasks that are often not attended to. The annual Russian Roulette of whose CPD (continual professional development) points will be audited when the time comes, is never pleasant to watch. The paradox that digitising electronic health records, should be making the healthcare professionals lives easier, is sadly ironic as it continues to attribute to physician burn out.
The amount of clerical and administrative work required for payers and other stakeholders, continues to compromise the patient. It results in less time with the patient and strangleholds what is left of the physician's autonomy and time.
As if this isn’t enough, there is also the obligatory industry airtime the HCPs are required to give:
* Sales reps in-practice
* The cumulative hours spent walking around industry exhibitions (whose headline acts are showers of branded pens)
* Publications oversaturated with advertisements (depending on the publication, one has to question the credibility of the journalism and editorials which, more and more, are reading suspiciously like advertorials).
These are just a few of the tactics in the pharmaceutical marketing arsenal, and after years of repetition, a lot of information portrayed is met with skepticism.
Across the board, the age-old model of pharmaceutical marketing is stale and uninspired in this day and age. However, budgets are needed for the support of the profession. The company that opts not to engage in these antiquated activities, appears more conspicuous by absence. It’s such a pity when there are more efficient ways to have meaningful conversations with clients - especially in the digital era.
HCPs are burnt out, information exchange is inefficient, and industry is not doing anything disruptive enough to shift the status quo.
Why is this industry, in particular, not embracing the information sharing and crowd-sourcing benefits of the digital age, that is enjoyed by so many other industries?
Digital Deep Dive
Beside the obvious PTSD of their ‘technology’ experiences with Electronic Health Records (EHRs), this conundrum has been hounding me. I heard the plight of the healthcare professional amidst the frustration of being a marketer in a space where there are significant budgets, enormous clout amongst established industry leaders, and less and less airtime with clients.
I have always taken on my professional role with my clients, products and teams as personally, and with the same anxious enthusiasm, as I would my own child. So I leapt into research, a lot of it. Being the millennial that I am (yes, I just make the cut!) I did a digital deep-dive. As you would imagine, there are some incredibly insightful pieces and conversations one can have in this digital age, when you ask the right questions, using the right platforms.
Which brings me to a statistic that completely took me aback. Recent research has revealed that almost 90% of hospitals in America still rely on pagers, considering them to be more secure, compared to smartphone-based communication. I read the same sentence over and over, until I was certain I hadn’t misread anything. Are we really using an analogue technology in the “mHealth” (Mobile Health) era?
The article goes on to clarify that outmoded modes of communication (like pagers) are far less efficient and estimated to cost US hospitals $8.3 billion a year in reduced productivity! Naturally, this then also impacts on quality of care as it takes away from the time that can be spent interfacing directly with patients. This not only highlights the inherently glacial pace of communication technology adoption in healthcare, but also represents an opportunity for new products that specifically address the unique challenges of the industry.
The majority of resources I identified for the clinician were primarily offline, however there were initiatives slowly coming online.
In South Africa, my stomping ground, there are conferences, journals, CPDs, and other resources taking these steps. They are not being executed especially well, and are happening at a snail’s pace, but at least there are websites and even social media pages, on existing public platforms. I saw a scary number of text heavy, WordPress websites, with poor user experiences, little detail, and easily hackable login portals (almost every login registration requirement being different from the next). I discovered a handful of apps, all with different siloed solutions, which creates a disjointed and confusing experience (and again, with differing login requirements).
Industry websites and apps are better developed and managed, however these always appear to be laden with the commercial agenda that their shareholders require. Understandably, as much as the Florence Nightingale persona establishes brand loyalty, there are commercial objectives to fulfil.
Still, it makes the HCP think before registering on a database that will be mined in exchange for the use of this service. I recently had a meeting with a significantly influential government body in the healthcare space. I was told that the application programming interface API (a software interface that allows applications to talk to each other) for their website is “still being developed” and has been at that stage for over a year. Sigh ...
So, from both the public and private sectors, I am not seeing a smooth transition to a more digitized healthcare ecosystem. The result is not surprising: Non-compliance - ironically, the term that makes every HCP shudder.
An international search reveals the contrast one would expect when comparing the digital developments of first-world and third-world countries. There are some amazing online tools that ‘get’ the digital revolution. The ubiquitous use of "Health Tech” and "Health 2.0” conjures up images of artificial intelligence (AI), virtual reality and intimidatingly ambitious tech devices that can diagnose, monitor, treat and even cure disease. There are already murmurings of the “Health 3.0” revolution.
And now?
But what about now? There is a proliferation of patient-centric technology, but what about the Healthcare Professionals? Where are the meaningful, cross-disciplinary conversations taking place? Why is everyone working in silos? Ironic, given the overuse of the word “Interoperability” – a buzz word that has been ‘making the rounds’ in the healthcare space for some time now – referring, for the most part, to EHRs. Although putting the letter “e” in front of already existing systems does technically make them “digital”, it doesn’t necessarily make them any more efficient or engaging.
Regardless of the reasons, which are complex and justifiable, this is me reaching out to those of you in this sphere, and the reason for what I am doing at MediFellows.
My purpose is to engage with those forward thinkers and digital leaders that are proactive in this space. Let’s exchange feedback, advice, mentorship, and more. I love the industry and my feet are strapped to the pedals on this one.
Published by: Fiona McGuirk
References:
https://www.physiciansweekly.com/wp-content/uploads/2016/08/frustrated-doctor-crazy-1080x663.png
https://www.forbes.com/sites/robertpearl/2019/07/08/physician-burnout-1/#f62ad8d119e8
https://www.capgemini.com/resources/digital-healthcare-survey/
https://www.siemens-healthineers.com/magazine/mso-pulse-plus-survey.html
https://rockhealth.com/why-doctors-still-use-pagers/
https://www.forbes.com/sites/dangingiss/2019/07/10/as-healthcare-goes-digital-consumer-engagement-and-experience-improve/#4996aeb496e6/
https://www.healthleadersmedia.com/clinical-care/3-takeaways-healthleaders-innovation-exchange
https://www.himss.org/news/current-state-interoperability
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5559244/
https://blogs.scientificamerican.com/observations/electronic-health-records-and-doctor-burnout/
Not only is the healthcare industry a digital laggard: riddled with inefficiencies; impersonal care, old technologies, and siloed digital approaches; it is also inherently averse to change – being highly regulated, with sensitivities around security and privacy of information.
I recently took to LinkedIn in an attempt to encourage meaningful communication between myself and like-minded professionals in the healthcare industry.
I was a rep once, so I eagerly searched the platform for my doctors, pharmacists and others I’d engaged with in the past... but, hardly anyone I searched for came up... Ok, well, I’d also engaged with numerous healthcare associations, institutions and practices in my marketing capacity, so I searched for these. Again, limited results…
I began to question my search method. The bottom line was a dismal attendance; not surprising, given the pace of the average Healthcare Professional’s (HCP) life.
Resource overload
As with any industry, an exchange of information is imperative. Time, by far, is the HCP’s most scarce resource, so it is understandable that it can become a nightmare when trying to determine which sources of information are the most meaningful and credible.
After all, we are bombarded with a multitude of options: conferences, CMEs, research, studies, journal clubs, websites, drug interaction checkers, acute and chronic medical aid references, prescription dosing, indications… the list goes on and on.
Then there is the time required for other administrative tasks that are often not attended to. The annual Russian Roulette of whose CPD (continual professional development) points will be audited when the time comes, is never pleasant to watch. The paradox that digitising electronic health records, should be making the healthcare professionals lives easier, is sadly ironic as it continues to attribute to physician burn out.
The amount of clerical and administrative work required for payers and other stakeholders, continues to compromise the patient. It results in less time with the patient and strangleholds what is left of the physician's autonomy and time.
As if this isn’t enough, there is also the obligatory industry airtime the HCPs are required to give:
* Sales reps in-practice
* The cumulative hours spent walking around industry exhibitions (whose headline acts are showers of branded pens)
* Publications oversaturated with advertisements (depending on the publication, one has to question the credibility of the journalism and editorials which, more and more, are reading suspiciously like advertorials).
These are just a few of the tactics in the pharmaceutical marketing arsenal, and after years of repetition, a lot of information portrayed is met with skepticism.
Across the board, the age-old model of pharmaceutical marketing is stale and uninspired in this day and age. However, budgets are needed for the support of the profession. The company that opts not to engage in these antiquated activities, appears more conspicuous by absence. It’s such a pity when there are more efficient ways to have meaningful conversations with clients - especially in the digital era.
HCPs are burnt out, information exchange is inefficient, and industry is not doing anything disruptive enough to shift the status quo.
Why is this industry, in particular, not embracing the information sharing and crowd-sourcing benefits of the digital age, that is enjoyed by so many other industries?
Digital Deep Dive
Beside the obvious PTSD of their ‘technology’ experiences with Electronic Health Records (EHRs), this conundrum has been hounding me. I heard the plight of the healthcare professional amidst the frustration of being a marketer in a space where there are significant budgets, enormous clout amongst established industry leaders, and less and less airtime with clients.
I have always taken on my professional role with my clients, products and teams as personally, and with the same anxious enthusiasm, as I would my own child. So I leapt into research, a lot of it. Being the millennial that I am (yes, I just make the cut!) I did a digital deep-dive. As you would imagine, there are some incredibly insightful pieces and conversations one can have in this digital age, when you ask the right questions, using the right platforms.
Which brings me to a statistic that completely took me aback. Recent research has revealed that almost 90% of hospitals in America still rely on pagers, considering them to be more secure, compared to smartphone-based communication. I read the same sentence over and over, until I was certain I hadn’t misread anything. Are we really using an analogue technology in the “mHealth” (Mobile Health) era?
The article goes on to clarify that outmoded modes of communication (like pagers) are far less efficient and estimated to cost US hospitals $8.3 billion a year in reduced productivity! Naturally, this then also impacts on quality of care as it takes away from the time that can be spent interfacing directly with patients. This not only highlights the inherently glacial pace of communication technology adoption in healthcare, but also represents an opportunity for new products that specifically address the unique challenges of the industry.
The majority of resources I identified for the clinician were primarily offline, however there were initiatives slowly coming online.
In South Africa, my stomping ground, there are conferences, journals, CPDs, and other resources taking these steps. They are not being executed especially well, and are happening at a snail’s pace, but at least there are websites and even social media pages, on existing public platforms. I saw a scary number of text heavy, WordPress websites, with poor user experiences, little detail, and easily hackable login portals (almost every login registration requirement being different from the next). I discovered a handful of apps, all with different siloed solutions, which creates a disjointed and confusing experience (and again, with differing login requirements).
Industry websites and apps are better developed and managed, however these always appear to be laden with the commercial agenda that their shareholders require. Understandably, as much as the Florence Nightingale persona establishes brand loyalty, there are commercial objectives to fulfil.
Still, it makes the HCP think before registering on a database that will be mined in exchange for the use of this service. I recently had a meeting with a significantly influential government body in the healthcare space. I was told that the application programming interface API (a software interface that allows applications to talk to each other) for their website is “still being developed” and has been at that stage for over a year. Sigh ...
So, from both the public and private sectors, I am not seeing a smooth transition to a more digitized healthcare ecosystem. The result is not surprising: Non-compliance - ironically, the term that makes every HCP shudder.
An international search reveals the contrast one would expect when comparing the digital developments of first-world and third-world countries. There are some amazing online tools that ‘get’ the digital revolution. The ubiquitous use of "Health Tech” and "Health 2.0” conjures up images of artificial intelligence (AI), virtual reality and intimidatingly ambitious tech devices that can diagnose, monitor, treat and even cure disease. There are already murmurings of the “Health 3.0” revolution.
And now?
But what about now? There is a proliferation of patient-centric technology, but what about the Healthcare Professionals? Where are the meaningful, cross-disciplinary conversations taking place? Why is everyone working in silos? Ironic, given the overuse of the word “Interoperability” – a buzz word that has been ‘making the rounds’ in the healthcare space for some time now – referring, for the most part, to EHRs. Although putting the letter “e” in front of already existing systems does technically make them “digital”, it doesn’t necessarily make them any more efficient or engaging.
Regardless of the reasons, which are complex and justifiable, this is me reaching out to those of you in this sphere, and the reason for what I am doing at MediFellows.
My purpose is to engage with those forward thinkers and digital leaders that are proactive in this space. Let’s exchange feedback, advice, mentorship, and more. I love the industry and my feet are strapped to the pedals on this one.
Published by: Fiona McGuirk
References:
https://www.physiciansweekly.com/wp-content/uploads/2016/08/frustrated-doctor-crazy-1080x663.png
https://www.forbes.com/sites/robertpearl/2019/07/08/physician-burnout-1/#f62ad8d119e8
https://www.capgemini.com/resources/digital-healthcare-survey/
https://www.siemens-healthineers.com/magazine/mso-pulse-plus-survey.html
https://rockhealth.com/why-doctors-still-use-pagers/
https://www.forbes.com/sites/dangingiss/2019/07/10/as-healthcare-goes-digital-consumer-engagement-and-experience-improve/#4996aeb496e6/
https://www.healthleadersmedia.com/clinical-care/3-takeaways-healthleaders-innovation-exchange
https://www.himss.org/news/current-state-interoperability
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5559244/
https://blogs.scientificamerican.com/observations/electronic-health-records-and-doctor-burnout/